Predictable Caries Removal with the Six Lessons Approach
As new materials and techniques are developed through dental research, the biggest hurdle is often replicating those findings in practice. Operator inconsistency is one of the leading causes of poor dental treatment outcomes, which means finding ways to increase predictability in every step of a restoration is key to achieving consistent restorative outcomes.
Protocols for predictable caries removal are especially helpful in cases with deep caries like this one by Dr. Davey Alleman, DMD.
Subjective caries removal vs objective caries removal
“…the determination of hardness by hand is an indefinite, subjective matter, and can never be an objective guide for caries removal. It is quite surprising that we dentists have, up to now, performed caries treatment, our most important professional duty, while relying on such an ambiguous means of detection which has no scientific basis.” - Dr. Takao Fusayama
This quote by Dr. Takao Fusayama, widely recognized as the father of adhesive dentistry, outlines the need for predictability in caries removal. While teaching caries removal to dental students, a student asked Dr. Fusayama “how hard is hard?” Students are taught to use a tactile approach, feeling for sound dentin, but this feeling will be different for every practitioner. This means the outcomes will be different for every practitioner too.
When relying on adhesion for a restoration, achieving consistent bonds is dependent on a consistent bonding field. If a practitioner is using subjective means of caries removal, like a tactile approach, they cannot guarantee the best possible bondable surface. Objective caries removal, one that does not vary between providers, is key to creating bonds to dentin that stay bonded for decades.
Here is the full case from Dr. Davey Alleman, DMD. Caries detector dye and central stop zone measurements are used to maximize the bond to dentin, even deep in the tooth.
Using caries detector dye (CDD) for objective caries removal
Dr. Takao Fusayama invented caries detector dye as a tool for objective caries removal. Caries detector dye becomes entrapped in denatured collagen from caries, showing exactly where caries is, and is not, in a tooth. Every practitioner who stains a tooth with caries detector dye will see the exact same stained and unstained areas of the tooth.
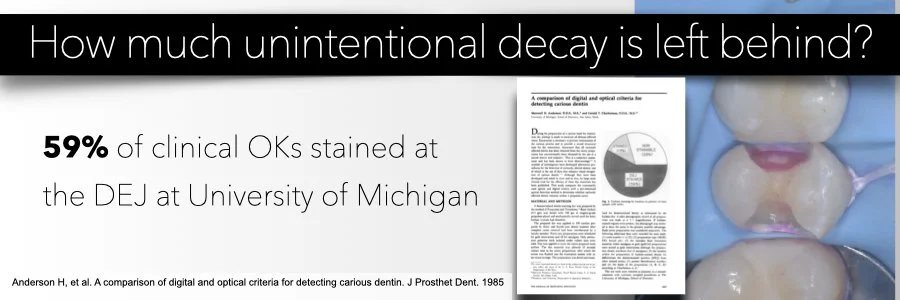
A 1985 study found that 59% of practitioners left caries behind when relying on a tactile, subjective approach, for caries removal. This is the easiest way to lose bond strength in an adhesive restoration, so moving to objective caries removal with caries detector dye will improve bond strengths in your restorations. (Anderson M, Charbeneau G. A comparison of digital and optical criteria for detecting carious dentin. J Prosth Dent. 1985;53(5): 643-646.)
Slide from the Biomimetic Mastership.
Partial caries removal to protect pulp vitality
A common misconception around caries detector dye is that using it requires complete caries removal in all cases. When creating his Six Lessons Approach, Dr. David Alleman outlined steps for partial caries removal for the following reasons:
Protecting pulp vitality: Partial caries removal, when paired with the peripheral seal zone concept for determining caries removal endpoints, prevents pulp exposures, which can increase a pulp’s risk of necrosis. By removing carious dentin in the bonding field and leaving carious dentin that is too close to the pulp to be safely removed without risk of exposure, you can maximize your bond strengths and protect the pulp.
Saving more teeth: Traditional techniques often recommend root canal therapy, crowns or extraction for teeth with deep caries. Thanks to advancements in adhesive dentistry, we are able to prevent this for vital teeth, even with deep caries. Deep caries is sealed with immediate dentin sealing, causing bacteria to become dormant and remineralization of demineralized dentin. This offers a more conservative treatment option compared to traditional recommendations.
This diagram from the 2012 paper by Drs. David Alleman and Pascal Magne outlines how caries removal stops to protect the pulp, which they called caries removal endpoints (CREs).
The peripheral seal zone and compression dome concepts
Predictable caries removal is only the first — but most important! — step in a long-lasting adhesive restoration. As outlined in Lesson 3 of the Six Lessons Approach, sealing the tooth at a strength that mimics the tooth’s natural connection to itself, 30-50 MPa, will stop new bacteria from entering under the restoration, giving the pulp a chance to heal. Bonding in the peripheral seal zone is supported by Graeme Milicich’s compression dome concept, which outlines how the strength of the tooth comes from its dome shape and hollow center around the pulp chamber — like a dome (Milicich G. The compression dome concept: the restorative implications. Gen Dent. 2017. 55-60.). If a biomimetic bond in the peripheral seal zone is achieved, the tooth will function like a natural tooth, even after deep caries treatment.
In this case by Dr. Davey Alleman, DMD, deep caries is left near the pulp to avoid pulp exposure. Six Lessons Approach protocols are used to seal the tooth at the nanometer level, preventing new bacteria from infecting the pulp and giving the pulp a chance to heal.
To learn the protocols for predictable caries treatment and bonding to dentin, view upcoming Alleman Center training programs. We offer in-person and online programs that cover every step in the Six Lessons Approach.
Learn more about best practices to avoid and treat pulp exposures in this Six Lessons Approach Podcast episode by Dr. David Alleman.